Abstract
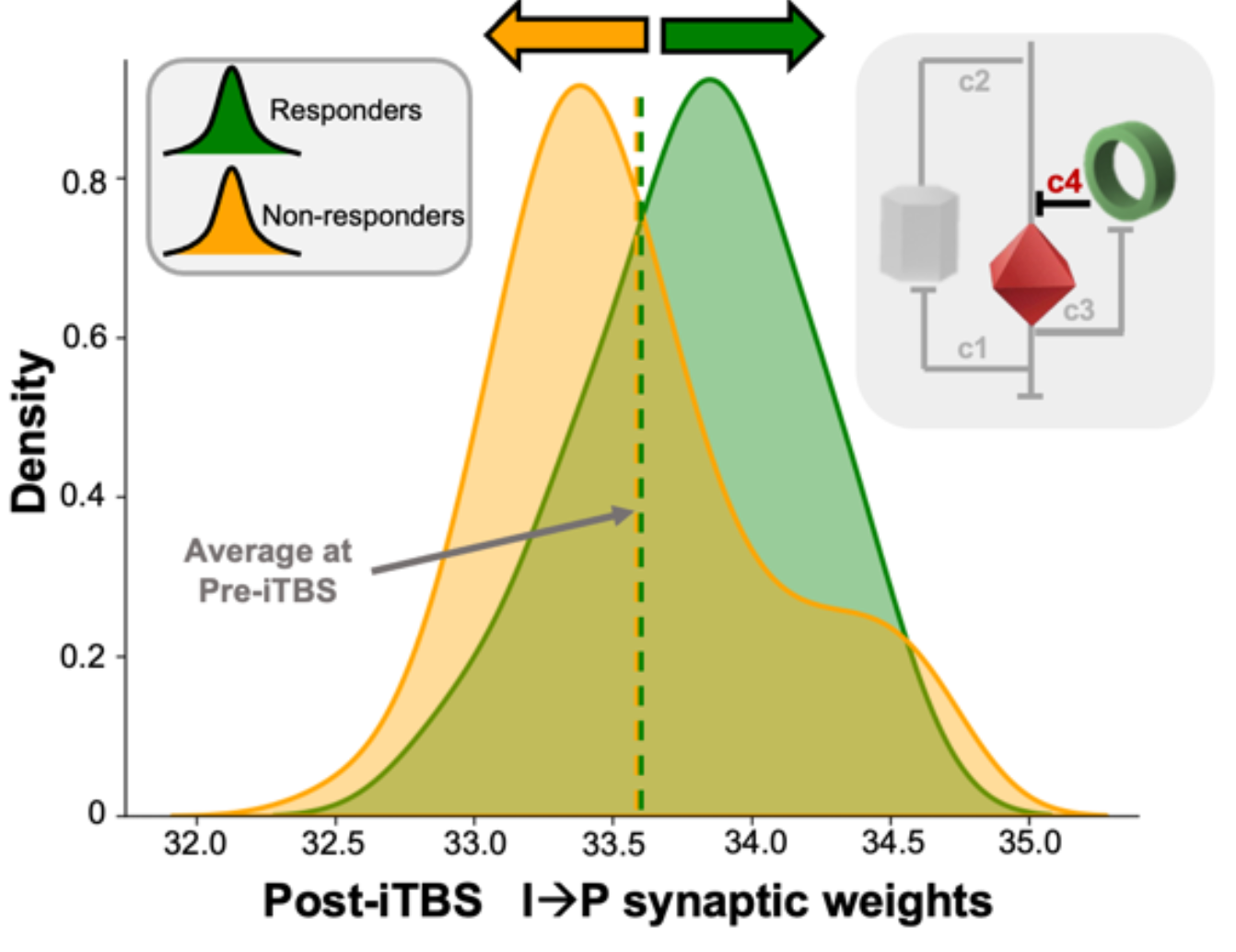
Depression affects over 350 million people worldwide, with treatment resistance occurring in up to 30% of cases. Intermittent theta burst stimulation (iTBS) targeting the left dorsolateral prefrontal cortex (DLPFC) has emerged as a promising intervention, yet the neurophysiological mechanisms determining which patients will respond remain poorly understood. Here, we combined transcranial magnetic stimulation with electroencephalography and whole-brain computational modeling to uncover the mechanistic basis of treatment efficacy in 90 patients with treatment-resistant depression. We identified two distinct neurophysiological signatures that differentiate responders from non-responders: (1) post-treatment shifts in excitation-inhibition balance toward greater inhibitory control, and (2) a pre-treatment brain state characterized by anticorrelated dynamics between subgenual anterior cingulate cortex and DLPFC. These features were significantly correlated with clinical improvement and could not be explained by non-specific factors. Our findings provide a neurophysiologically-informed framework for developing personalized and optimized neuromodulation approaches in treatment-resistant depression.