Abstract
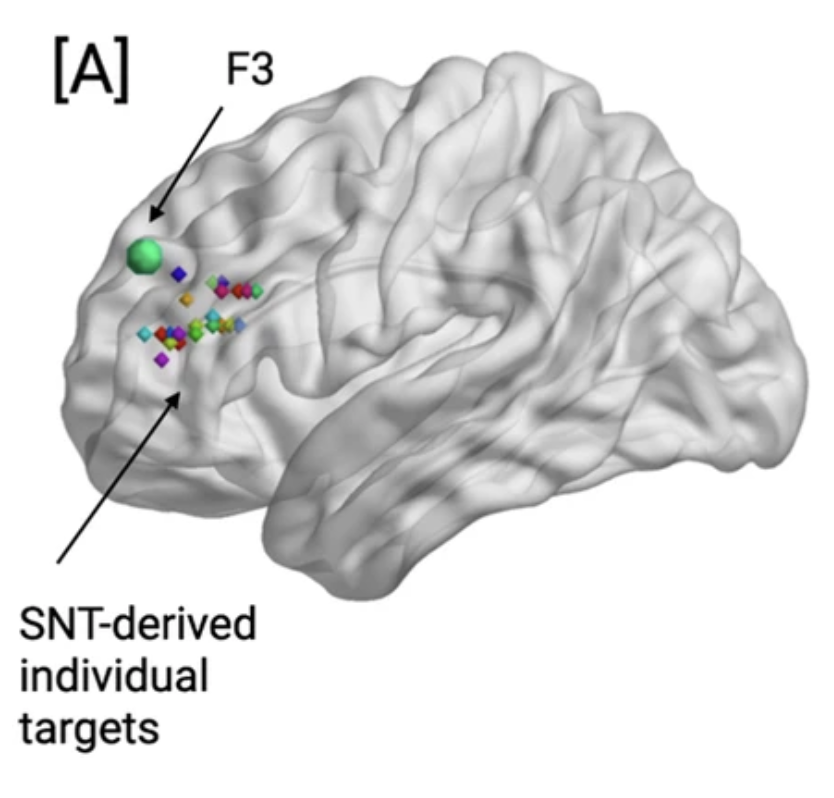
SNT is a high-dose accelerated intermittent theta-burst stimulation (iTBS) protocol coupled with functional-connectivity-guided targeting that is an efficacious and rapid-acting therapy for treatment-resistant depression (TRD). We used resting-state functional MRI (fMRI) data from a double-blinded sham-controlled randomized controlled trial1 to reveal the neural correlates of SNT-based symptom improvement. Neurobehavioral data were acquired at baseline, post-treatment, and 1-month follow-up. Our primary analytic objective was to investigate changes in seed-based functional connectivity (FC) following SNT and hypothesized that FC changes between the treatment target and the sgACC, DMN, and CEN would ensue following active SNT but not sham. We also investigated the durability of post-treatment observed FC changes at a 1-month follow-up. Study participants included transcranial magnetic stimulation (TMS)-naive adults with a primary diagnosis of moderate-to-severe TRD. Fifty-four participants were screened, 32 were randomized, and 29 received active or sham SNT. An additional 5 participants were excluded due to imaging artifacts, resulting in 12 participants per group (Sham: 5F; SNT: 5F). Although we did not observe any significant group × time effects on the FC between the individualized stimulation target (L-DLPFC) and the CEN or sgACC, we report an increased magnitude of negative FC between the target site and the DMN post-treatment in the active as compared to sham SNT group. This change in FC was sustained at the 1-month follow-up. Further, the degree of change in FC was correlated with improvements in depressive symptoms. Our results provide initial evidence for the putative changes in the functional organization of the brain post-SNT.